Veterans and PTSD: The Ongoing Battle

The Mental and Emotional
Aftermath of War
In February 2015, Iraq War veteran Richard Miles entered a VA hospital in Des Moines, Iowa, and told the staff: “I need help.”
This wasn’t his first visit to the Iowa VA. Between 2008 and 2009, Miles had been admitted four times after two unsuccessful suicide attempts.
This time, he was diagnosed with “worsened PTSD,” anxiety and insomnia. He assured the staff that he was not a harm to himself, but “I do need some medicine so I can just rest.” He was given the medication that had helped him in the past.
Five days later, Miles was found frozen to death in the woods, having consumed a toxic amount of the pills. He was 40 years old.
Every Veterans Day, we celebrate the brave individuals who have served our country through the armed forces. For many of them, however, the mental and emotional warfare continues long after they've left the physical battlefield behind.
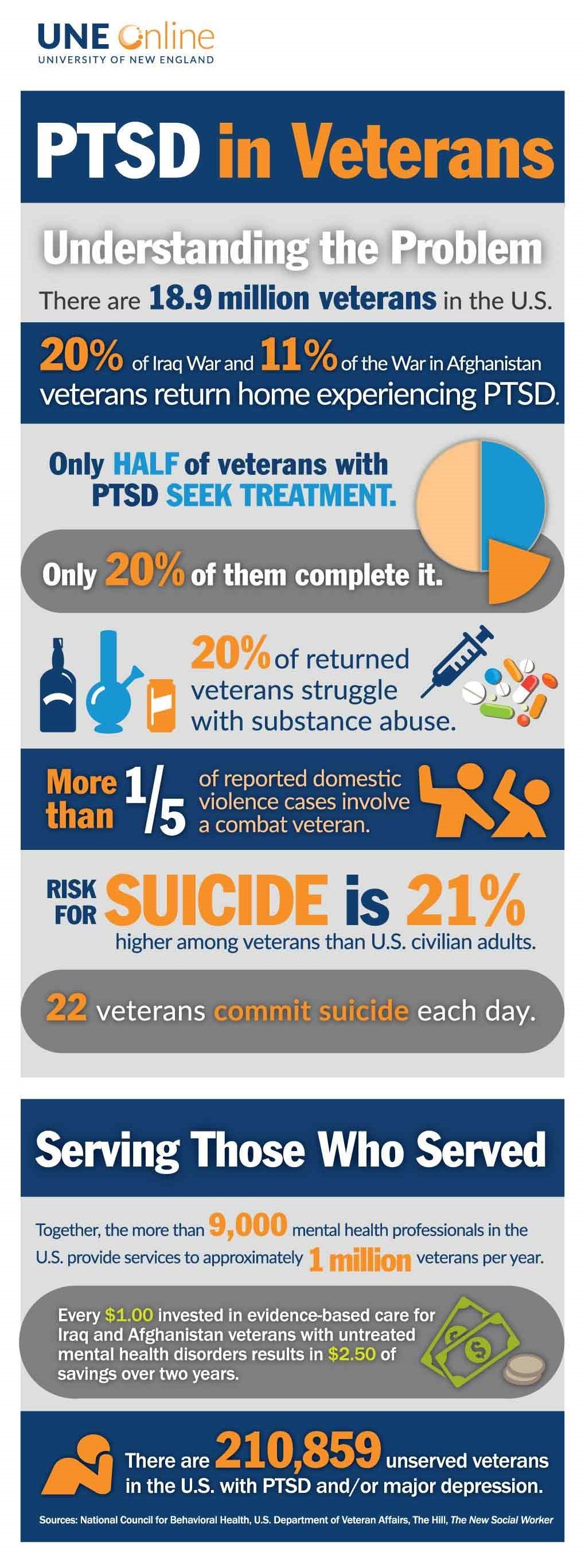
Recent studies indicate that almost 16% of U.S. veterans will experience PTSD at some point in their lives, compared to a 9% PTSD rate for the general population. (See sidebar, "PTSD by Service Era.”) In addition, veteran suicide rates hover around 35% -- more than double the 15% rate for non-veterans.
Regional Differences
U.S. states vary widely in the PTSD rate among their military veterans, from 9.9% (Alaska) to 3.8% (Hawaii). Military and governmental authorities offer several reasons for this discrepancy:

PTSD by Service Era
The following table outlines PTSD rates for U.S. veterans engaged in military conflicts since WWII:
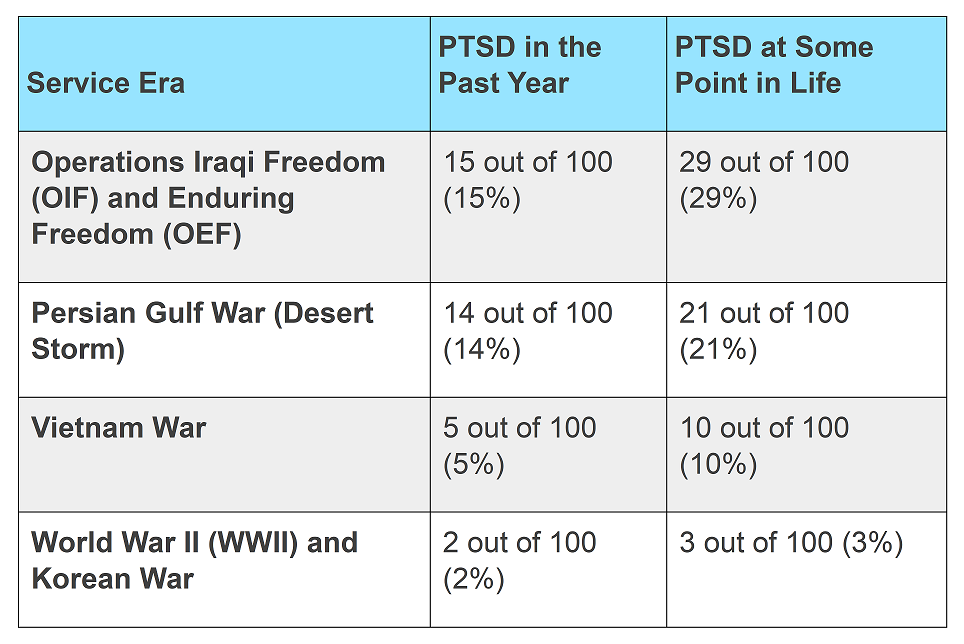
Source: VA National Center for PTSD
Veteran Demographics
States with more post-9/11 vets (such as Alaska, New Mexico, and Wyoming) see higher PTSD rates. According to Mission Roll Call, younger combat veterans, especially those who served multiple tours, are much more likely to carry psychological trauma than older, peacetime veterans.
Access to Mental Health Care
Mental health care is not always accessible in remote or rural areas. While telehealth is helping to bridge that gap, broadband access remains spotty in many rural areas.
Stigma and Culture
In tight-knit rural or traditional communities, veterans suffering from PTSD can be encouraged to "tough it out." Dissuaded from talking about mental health or seeking treatment, their PTSD goes untreated.
Screening and Reporting Practices
Some government sources indicate that VA-heavy states, such as Rhode Island and Massachusetts, may be detecting more PTSD cases early or offering better support. Other states may underreport PTSD because of cultural or logistical barriers.
Ways You Can Help
Here are four key ways to lend support to PTSD victims suffering from the aftermath of combat.
1. Listen
If the veteran wants to talk about what they experienced, encourage them to do so. Give them your full attention, maintain a non-judgmental attitude, and don't rush them.
Keep your questions unintrusive. Avoid offering advice or opinion unless asked.
2. Build Social Support
Social withdrawal is a common symptom among veterans struggling with PTSD. Encourage the veteran to maintain other relationships, participate in social activities, and confide in at least one other safe individual.
3. Create a Sense of Safety
Stability is essential for veterans with PTSD. Take care to provide a consistent, steady presence in the veteran's life.
The timing of recovery is a personal matter for each individual, so be sure to respect the veteran's privacy. Treat everything they tell you as completely confidential (unless you're genuinely afraid they're about to harm themself or another person).
4. Encourage Specialized Treatment
Finally, encourage the veteran to seek out and enroll in specialized treatment for military PTSD.
--Article Continues Below--
Treatment Options
Proper mental health care can not only minimize the symptoms but also reduce the long-term risk of developing additional health conditions. Many treatment options for PTSD in veterans are available:
- Medication for anxiety and depression
- Counseling and talk therapy, including:
- Chemical dependency detox for individuals struggling with addiction or substance use
- Holistic treatment, such as meditation, mindfulness, acupuncture, music, or pet therapy
In-person and online mental health services are available through the VA.
Ensuring Proper Diagnosis
Military veterans deserve our support. Unfortunately, PTSD is often underdiagnosed or misdiagnosed. The website Tethered to PTSD is designed exclusively for healthcare professionals, providing the resources they need to identify probable PTSD in a primary care setting.
Sources:
Featured Image: Adobe, License Granted
CNN
VA National Center for PTSD
Recent Posts










Share On: